Scientific Calendar March 2020
Treatment of venous thromboembolism (VTE) in cancer patients
What is the standard of care for treatment of acute cancer associated thrombosis?
Low-molecular-weight heparin (LMWH)
Direct oral anticoagulants (DOACs, e.g. apixaban)
Vitamin K antagonists (VKA)
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Scientific background
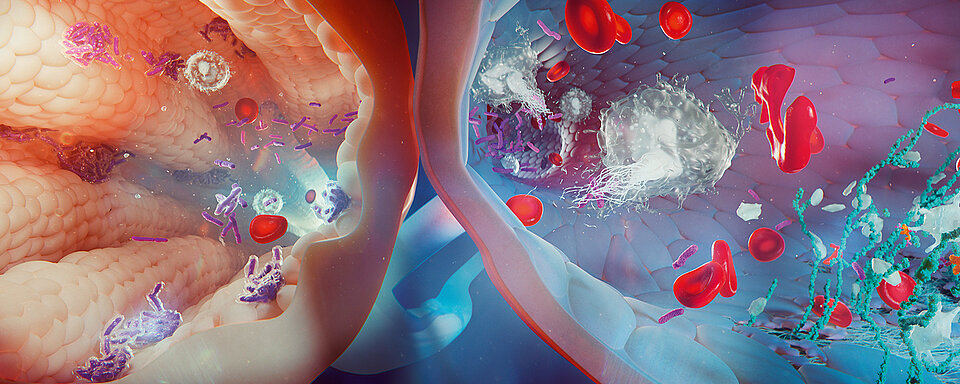
Cancer patients have a significantly higher risk of developing venous thromboembolism (VTE) in comparison to individuals without cancer. The higher risk is caused by various factors, e.g. the cancer itself, treatment-related and patient-related factors, and their combination. [1] The optimal prevention and treatment of VTE are essential parts of patient care because patients with cancer-associated thrombosis (CAT) have significantly shorter overall survival than cancer patients without thrombosis. Inadequate VTE prevention and treatment may have impact on the quality of life, delay cancer treatment or lead to complications such as recurrent VTE and/or bleeding.
Several trials have investigated the optimal treatment for the primary prevention of thrombosis in cancer patients. Patients with active or recently diagnosed cancer who are admitted to hospital should receive thromboprophylaxis during their hospital stay unless clinically contraindicated. Outpatients with active cancer should be assessed for thrombosis risk and, although most do not routinely require thromboprophylaxis, should be considered high risk patients in general. Routine use of anticoagulants at prophylactic or therapeutic dose is not recommended to prevent catheter-related thrombosis in cancer patients and patients without a history of VTE receiving adjuvant hormonal therapies for cancer because thromboprophylaxis does not reduce the risk of VTE significantly. [2]
Recent data has demonstrated a significant reduction of deep vein thrombosis (DVT) events in cancer patients undergoing perioperative pharmacological thromboprophylaxis compared to cancer patients without prophylaxis. The data showed that the risk of bleeding events remains acceptable and without differences in mortality and pulmonary embolism. [3] The risk of VTE is further reduced by extending the thromboprophylaxis up to 2-6 weeks after certain cancer surgeries (e.g. abdominal and pelvic surgery). [4, 5]
Low-molecular-weight heparin (LMWH) has been the standard of care for treatment of acute CAT for decades and is recommended in all major guidelines for the prophylaxis of hospitalised patients with active cancer. [6-8] However, the guidelines do not recommend their use for routine VTE prophylaxis for all cancer outpatients. Only in very high risk VTE patients (e.g. stomach, pancreas, lung, testicular cancer and lymphoma patients) should LMWH treatment be considered in general. [6-9] Compared to vitamin K antagonists (VKA), LMWH reduces the risk of recurrent VTE by no elevated risk of major bleeding events. Patients with CAT treated with LMWH for 6 months have a significantly lower VTE recurrence rate at 6 months than CAT patients under conventional treatment with VKA. [10-12] Therapeutic dose LMWH must be considered carefully in patients with renal impairment, because there is evidence of a higher prevalence of major bleeding events in patients with renal failure compared with those with normal renal function. [13] This may lead to dose reduction or the need of anti-Xa monitoring.
An alternative to LMWH in cancer patients with long-term treatments might be oral anticoagulant therapy if the patient does not wish to continue with daily injections needed with LMWH after 6 months. Direct oral anticoagulants (DOACs) were introduced in 2008. There are five DOACs currently on the market, but only four DOACs have been approved for the treatment of DVT and/or PE in Europe: dabigatran, rivaroxaban, apixaban and edoxaban. All have demonstrated a comparable efficacy and safety to VKA in cancer patients, but patients undergoing DOAC treatment have lower risks of both recurrent VTE and bleeding. [14, 15]
Recent published data comparing efficacy and safety of DOACs with LMWH in cancer patients are positive. DOACs are at least as effective as LMWH for the prevention of recurrent VTE, but increase the risk of major bleeding, mainly gastrointestinal. However, the severity of bleeding is less in patients treated with DOACs. [16, 17]
VKA should be a ‘third choice’ for cancer patients and used in situations where neither a DOAC nor LMWH only is feasible. VKA are less effective than LMWH in the prevention of recurrent cancer-associated VTE, having slow onset and offset, interactions with drugs and diet and requiring frequent laboratory monitoring and dose adjustment. [18] Therefore, even though still widely used in patients with CAT, VKA treatment is not strongly recommended as the preferred treatment for CAT in major guidelines. [19]
References
[1] Prandoni P., Lensing A.W.A., Piccioli A. et al. Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosis. Blood 2002;100(10):3484–88.
[2] Watson et al. Guideline on aspects of cancer-related venous thrombosis. British Journal of Haematology, 2015, 170, 640–648.
[3] Guo Q, Huang B, Zhao J, et al. Perioperative pharmacological thromboprophylaxis in patients with cancer: a systematic review and meta-analysis. Ann Surg. 2017;265:1087–93.
[4] Fagarasanu A, Alotaibi GS, Hrimiuc R, Lee AY, Wu C. Role of extended thromboprophylaxis after abdominal and pelvic surgery in cancer patients: a systematic review and meta-analysis. Ann Surg Oncol. 2016;23:1422–30.
[5] NICE. Venous thromboembolism: reducing the risk: reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in patients admitted to hospital. Clinical Guideline 92. National Institute for Health and Clinical Excellence, London. 2010.
[6] Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149:315–52.
[7] Lyman GH, Bohlke K, Falanga A, et al.; American Society of Clinical Oncology. Venous thromboembolism prophylaxis and treatment in patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Oncol Pract. 2015;11:e442–4.
[8] Streiff MB, Holmstrom B, Ashrani A, et al. Cancer-associated venous thromboembolic disease, version 1.2015. J Natl Compr Canc Netw. 2015;13:1079–95.
[9] Mandale et al. Management of venous thromboembolism (VTE) in cancer patients: ESMO Clinical Practice Guideline. Ann Oncol 2011.; 22 Suppl 6:vi85-92.
[10] Lee et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. New England Journal of Medicine. 2003; 349, 146–153.
[11] Meyer et al. Comparison of low-molecular-weight heparin and warfarin for the secondary prevention of venous thromboembolism in patients with cancer: a randomized controlled study. Archives of Internal Medicine. 2002; 162, 1729–1735.
[12] Hull et al. Long-term low-molecular-weight heparin versus usual care in proximal-vein thrombosis patients with cancer. American Journal of Medicine, 119, 1062–1072.2006.
[13] Hetzel et al. The heparins: all a nephrologist should know. Nephrology Dialysis Transplantation, Volume 20, Issue 10, October 2005, Pages 2036–2042.
[14] Vedovati et al. Direct oral anticoagulants in patients with VTE and cancer: a systematic review and meta-analysis. Chest. 2015;147:475–83.
[15] Carrier et al. Efficacy and safety of anticoagulant therapy for the treatment of acute cancer-associated thrombosis: a systematic review and meta-analysis. Thromb Res. 2014;134:1214–9.
[16] Li et al. Direct oral anticoagulant (DOAC) versus low-molecular-weight heparin (LMWH) for treatment of cancer associatd thrombosis (CAT): a systemic review and meta-analysis. Thromb Res. 2018. https://10.1016/j.thromres.2018.02.144. thromres.2018.02.144.
[17] Young A.M., Marshall A., Thirlwall J. et al. Comparison of an oral factor Xa inhibitor with low molecular weight heparin in patients with cancer with venous thromboembolism: results of a randomized trial (SELECT-D). J Clin Oncol. 2018;36(20):2017–23.
[18] Lee, A.Y. Treatment of established thrombotic events in patients with cancer. Thrombosis Research, 129(Suppl 1) 2012, S146–S153.
[19] Khorana et al. Current practice patterns and patient persistence with anticoagulant treatments for cancer-associated thrombosis. Res Pract Thromb Haemost. 2017;1:14–22.