Scientific Calendar July 2019
How can haematology analysers of the XN-Series support in detecting red blood cell disorders?
By detecting an increased MCHC value and subsequent triggering of the CBC-O App, which, in case of a positive RBC score, will propose a peripheral blood smear.
By detecting an increased MCHC value and subsequent triggering of the CBC-O App, which, in case of a negative RBC score, will propose a peripheral blood smear.
By detecting an increased MCHC value alone.
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Scientific Background
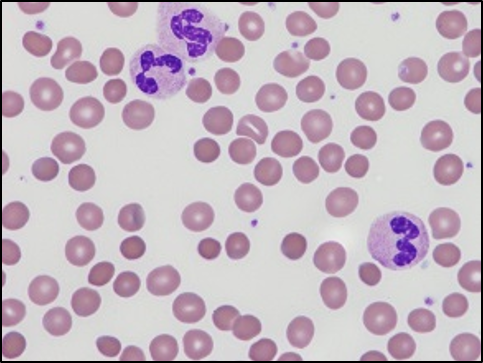
Hereditary spherocytosis (HS) is a pathologic condition that affects red blood cells. This inherited disorder is caused by mutations in genes involved in the synthesis of membrane proteins, and because of these dysfunctional membrane proteins, the red blood cells change their shape. The abnormal red cells are sphere-shaped rather than showing a normal biconcave disk shape. The difference in shape makes these red blood cells less flexible and more fragile [1]. These abnormal spherocytes are degraded in the spleen, leading to extravascular haemolysis. The disease is most common in European and North American Caucasian and Japanese populations with an incidence of 1 in 5,000 births, with several cases due to spontaneous mutations.
The clinical picture of the disease may range from symptom-free carriers to patients with a mild, moderate or severe form of HS. Symptoms of the disease are typically jaundice, splenomegaly and ‒ sometimes ‒ anaemia. Patients can develop gallstones, due to the bilirubin of the degraded cells, which accumulates in the gall bladder. People with the moderate-to-severe form of HS show all the features of the moderate form, but additionally have severe anaemia, which requires frequent blood transfusions to replenish their red blood cell supply. These patients also have severe splenomegaly and jaundice and are at a high risk of developing gallstones.
A special group are carriers of the mild form of hereditary spherocytosis without clinical symptoms and with a positive family history. In these individuals, incidental conspicuous laboratory results can be found. The normal CBC with a slightly elevated MCHC (mean cellular haemoglobin concentration) value is of special relevance to identify certain patients with RBC membrane diseases including HS. In such cases, the elevated MCHC can be the first indicative sign leading to a peripheral blood smear and the detection of spherical red blood cells.
Managing increased MCHC in daily routine practice
Although an elevated MCHC is quite a rare event in routine laboratory practice, it must be managed properly. It may be just an analytical artefact or referring to a truly pathological sample. Measurement abnormalities related to one or more of the following parameters ‒ red blood cells (RBC), haemoglobin (HGB), mean cell volume (MCV) or haematocrit (HCT) ‒ lead to abnormal RBC indices, especially the MCHC. In fact, different causes lead to spurious results of RBC, HCT or HGB measurements ‒ for instance, the presence of antibodies causing RBC agglutination (cold agglutinins) or abnormal plasma (lipaemic, haemolytic or icteric condition, or abnormal protein). An increased MCHC in its true clinical sense can be seen in case of acquired or hereditary disorders ‒ a modification of the red blood cell volume homoeostasis is observed with dehydration. Water loss generates a decreased cell volume and an increased haemoglobin concentration [2]. In rare cases, a truly increased MCHC due to dehydrated RBC can be found in patients with severe ionic troubles or those who have been treated with certain drugs [3].
The laboratory’s challenge is to determine the cause of the increased MCHC.The CBC-O concept implemented in the Extended IPU helps laboratories to resolve the problem caused by the interferences in traditional CBC measurement methodologies. When the MCHC is increased, CBC-O ensures that a RET channel reflex measurement is performed automatically. After the measurement generating the optical parameters from the RET channel, a dedicated algorithm [4] is applied to identify the cause behind the increased MCHC (cold agglutination, lipaemia, haemolysis, RBC disease, etc.) and proposes a corrective action to the user. This way, the analyst can decide to report the best possible CBC result. As part of the CBC-O concept, an RBC score (based on RET and FRC parameters) is calculated and, when positive, a blood smear to observe RBC morphology is recommended for the sample in question. The RBC score has been found to allow highly sensitive detection of RBC disease, which can actually help to speed up the diagnosis of RBC disorders such as hereditary spherocytosis [4].
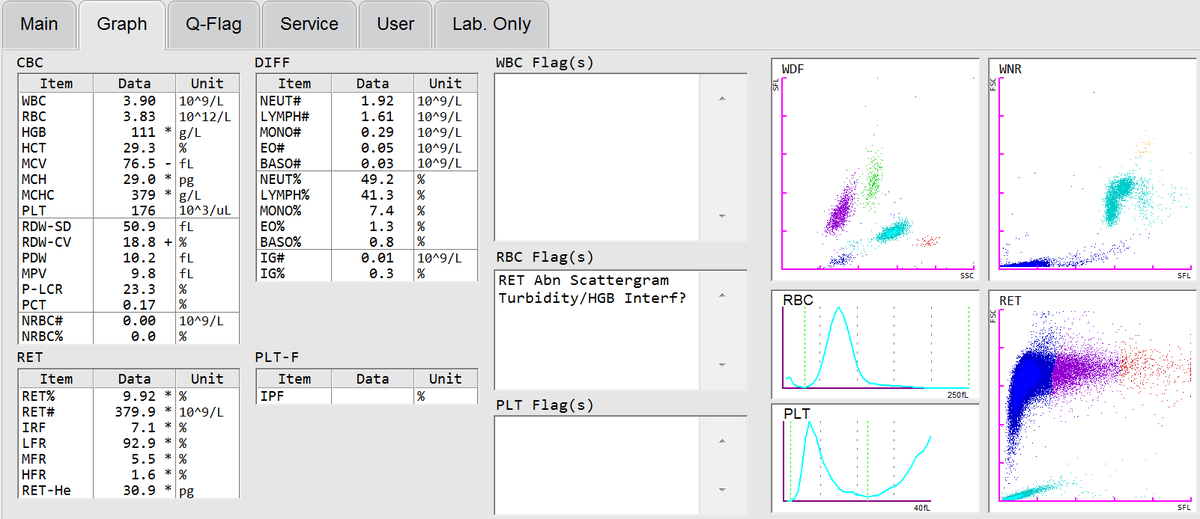
In case of a 14-year-old boy with severe abdominal pain, a complete blood count that was performed on a Sysmex XN analyser revealed a mild anaemia, normal WBC and PLT counts and an increased MCHC (Fig. 1).
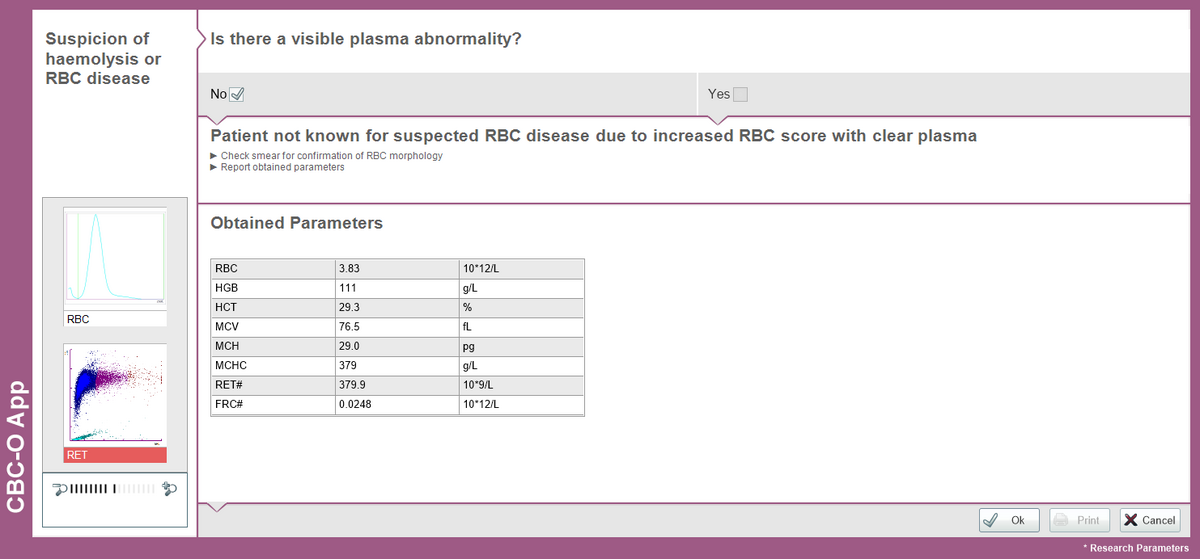
Due to the increased MCHC value, the CBC-O App was triggered (Fig. 2) and a positive RBC score revealed that the MCHC value was truly increased, which could be caused by RBC disease or haemolysis.
The plasma was clear without any visible abnormality and, since the patient was not known for having RBC disease, the laboratory consequently performed a peripheral blood smear in which spherical red blood cells were detected (Fig. 3).
Graphics
References
[1] Cotran RS et al. (2005) Robbins and Cotran pathologic basis of disease. Elsevier Saunders. p. 625. ISBN 0-7216-0187-1.
[2] Gallagher PG. (2013) Disorders of red cell volume regulation. Curr Opin Hematol. 20(3):201-7.
[3] Godon A et al. (2012) Automated hematology analysers and spurious counts Part 3. Haemoglobin, red blood cells, cell count and indices, reticulocytes. Ann Biol Clin (Paris). 70(2):155-68.
[4] Berda-Haddad Y et al. (2017) Increased mean corpuscular haemoglobin concentration: artefact or pathological condition? Int J Lab Hematol. 39(1):32-41.