Scientific Calendar May 2020
Does the immature platelet count (IPF#) provide any insights into antiplatelet therapy in patients with cardiovascular disease?
No, there is no scientific evidence for a correlation between IPF# and the response to antiplatelet therapy.
Yes, an increased IPF# is strongly associated with increased residual platelet reactivity and reduced response to aspirin, clopidogrel and prasugrel, but not to ticagrelor.
Yes, an increased IPF# is associated with increased residual platelet reactivity and reduced response to ticagrelor.
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Scientific background
This month’s calendar case presents a clinical case demonstrating recurrent cardiovascular events despite antiplatelet therapy (aspirin and/or clopidogrel) in a patient with accelerated platelet turnover. The patient’s clinical outcome normalised after shifting to ticagrelor [1].
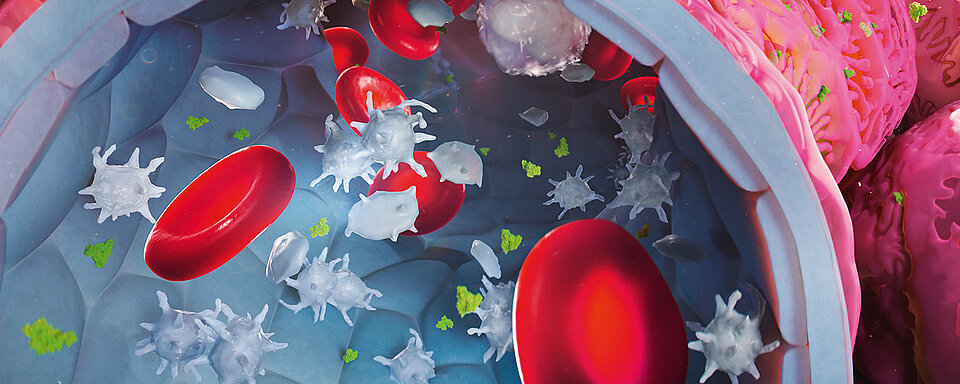
Clopidogrel is a widely used antiplatelet drug in the treatment and prevention of cardiovascular diseases. The drug irreversibly inhibits the P2Y12 receptor, thus inhibiting platelet aggregation and reducing the risk of adverse cardiovascular events [2]. However, under clopidogrel treatment, recurrent cardiovascular events remain a significant cause of morbidity and mortality [3]. This may be partly explained by a reduced platelet inhibition in response to clopidogrel [4]. Therefore, more potent P2Y12 antagonists have been developed to improve platelet inhibition. In patients suffering from myocardial infarction or stroke and after percutaneous coronary intervention, ticagrelor provides stronger and more consistent platelet inhibition compared with clopidogrel [2,5].
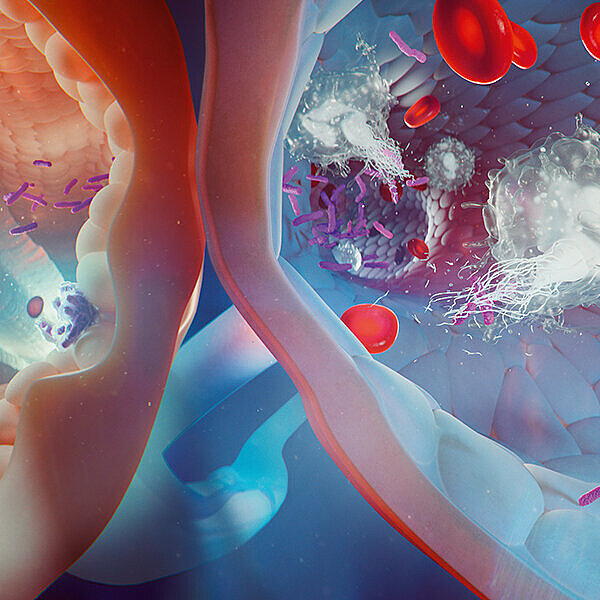
A 58-year-old man presented with symptoms and signs of cerebral infarction. His medical history included five previous ischaemic strokes, as well as carotid artery disease. His cardiovascular risk factors included hypertension, hypercholesterolaemia and smoking. Three years earlier, he had been diagnosed with polycythaemia vera (PV) with concomitant thrombocytosis. His usual treatment included clopidogrel monotherapy 75 mg once daily, which had been chosen instead of aspirin due to his comprehensive thrombosis history. A magnetic resonance imaging scan showed new infarctions in the vermis and left cerebellar hemisphere. Haematological parameters included a platelet count of 890 ×109/L, white blood cells 22.1 ×109/L, and a haematocrit of 0.47 L/L. The patient was successfully treated with tissue plasminogen activator 90 mg according to weight. At discharge, he was prescribed dual antiplatelet therapy (DAPT) consisting of clopidogrel and aspirin, both 75 mg once daily for three months followed by clopidogrel monotherapy. Treatment of his PV disease was intensified with cytoreductive treatment (hydroxyurea) and venesection.
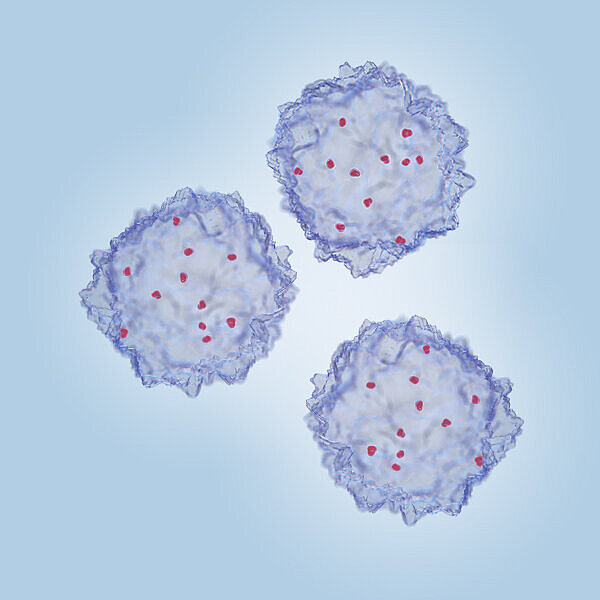
Five months after discharge and only two months after the patient stopped taking aspirin, he was admitted with ST-segment elevation myocardial infarction (STEMI). In the acute phase, he received standard loading DAPT, consisting of aspirin 300 mg and ticagrelor 180 mg, as well as intravenous heparin 10,000 IU. Acute coronary angiography showed complete occlusion of the right coronary artery. He underwent coronary stenting, and DAPT was continued with aspirin 75 mg once daily and ticagrelor 90 mg twice daily. Echocardiography showed a left ventricular ejection fraction of 50 % with akinesia corresponding to the supply area of the right coronary artery. The cardiologists observed an increased platelet count, immature platelet count (IPF#), and immature platelet fraction (IPF) three days after STEMI: the platelet count was at 682 ×109/L, IPF# at 25.9 ×109/L (reference range: 2.5–16.6) and IPF at 3.8 % (reference range: 1.1–6.1) [1]. Platelet aggregation was simultaneously analysed using whole blood aggregometry, demonstrating increased platelet aggregation in response to ADP and arachidonic acid despite treatment with aspirin and ticagrelor. Seventeen days later, IPF#, IPF, and arachidonic acid-induced platelet aggregation decreased, but ADP-induced platelet aggregation remained increased. DAPT was continued with aspirin 75 mg once daily and ticagrelor 90 mg twice daily. Since then (12 months), no cardiovascular event has been reported.
Patients with PV have a high risk of thromboembolic complications, but the mechanisms of thrombosis are not fully understood. The hyper-viscosity syndrome associated with most chronic myeloproliferative syndromes may be important, and other suggested mechanisms include an overactive JAK/STAT pathway. The present case report suggests that antiplatelet treatment in these patients may not have the expected protective effects. Our patient suffered six episodes of cerebral infarction and one episode of STEMI, despite the initial treatment with clopidogrel. During this period, the patient had a home nurse to confirm optimal compliance with medications. Following the last event of ischaemic stroke treated with thrombolysis, his antiplatelet treatment was changed for a three-month period to dual therapy. After that, the patient was switched back to clopidogrel monotherapy, and only two months later, he experienced STEMI. The antiplatelet treatment was then intensified again with aspirin 75 mg once daily and ticagrelor 90 mg twice daily. It is difficult to determine the exact reasons for the insufficient platelet inhibition. However, a plausible explanation may be an accelerated platelet turnover. IPF# and IPF were measured as a marker of increased platelet turnover and showed increased values three days after STEMI. The patient had thrombocytosis and was a smoker, factors which are both known to be associated with an accelerated platelet turnover. In patients with accelerated platelet turnover, an increased proportion of immature platelets are released from the bone marrow. These immature, reticulated platelets seem to be more reactive in a haemostatic way. They can produce proteins involved in haemostasis, due to residual mRNA derived from megakaryocytes, and are therefore more likely to participate in thrombus formation [6,7]. Seventeen days after the myocardial infarction, the cardiologists observed a decrease in IPF, but the values were still above the reference interval, being consistent with accelerated platelet turnover in a more stable phase. In addition to very high platelet counts, continually high values of IPF were found. Our patient’s poor response to clopidogrel may therefore partly be explained by an accelerated platelet turnover, counteracting the antiplatelet effects of clopidogrel. The poor response may also partly be a consequence of thrombocytosis.
In conclusion, patients with PV have a high risk of thromboembolic complications. Exploring mechanisms of thrombosis in these patients is important, and this case report illustrates that poor response to antiplatelet therapy may be a contributing factor. IPF# and IPF can be used as markers of accelerated platelet turnover and poor response to antithrombotic treatment.
References
[1] Pedersen OH et al. (2017) Recurrent Cardiovascular Events Despite Antiplatelet Therapy in a Patient with Polycythemia Vera and Accelerated Platelet Turnover. Am J Case Rep. 18:945–8.
[2] Grove EL et al. (2015) Antiplatelet therapy in acute coronary syndromes. Expert Opin Pharmacother. 16(14):2133–47.
[3] Wurtz M et al. (2013) Pharmacogenomics in cardiovascular disease: Focus on aspirin and ADP receptor antagonists. J Thromb Haemost. 11(9):1627–39.
[4] Yudi M et al. (2016) Clopidogrel, prasugrel or ticagrelor in patients with acute coronary syndromes undergoing percutaneous coronary intervention. Intern Med J. 46(5):559–65.
[5] Wallentin L et al. (2009) Ticagrelor versus clopidogrel in patients with acute coronary syndromes. New Engl J Med. 361(11):1045–57.
[7] Armstrong PC et al. (2017) Newly Formed Reticulated Platelets Undermine Pharmacokinetically Short-Lived Antiplatelet Therapies. Arterioscler Thromb Vasc Biol. 37(5):949–56.