Scientific Calendar February 2019
How can fluorescence flow cytometry (FFC) support the differential diagnosis of haematuria?
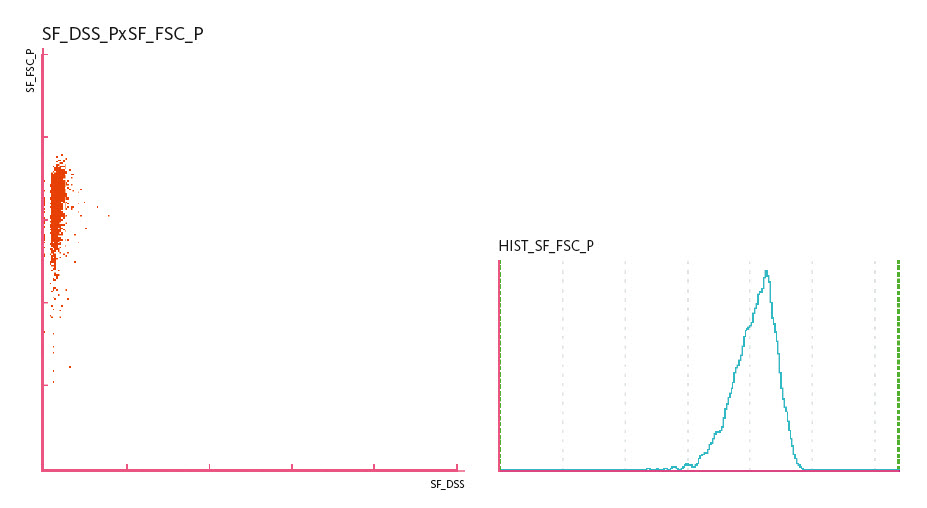
An 80-year-old male was examined during a regular check-up for managing his diabetes mellitus. Micro-haematuria was found and FFC examination of the urine indicated that the red blood cells (RBC) were isomorphic, in keeping with non-glomerular bleeding. Urine cytology was performed, which revealed cancerous cells of urothelial origin.
Haematuria is defined as the presence of RBC in urine. Causes can be categorised into glomerular, i.e. arising from the kidney, or non-glomerular causes. The latter include urinary tract infection or urinary tract calculi, whereby blood vessels damaged due to these causes leak directly into the urinary tract. As such, this type of haematuria is characterised by isomorphic RBC, which appear as a distinctive population in FFC. Occasionally, as is the case here, non-glomerular haematuria can also be caused by cancer of the urinary tract.
ISOMORPHIC RBC
Which statement is true for isomorphic RBC?
Their presence indicates glomerular haematuria.
They often vary in size and shape, sometimes with inner and outer vesicle-like protrusions.
They mostly appear as round or biconcave cells with a smooth surface and are uniform in size.
Isomorphic RBC are only observed in patients with persistent macrohaematuria.
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Scientific Background Information
Urinalysis is an effective method to detect kidney or urinary tract diseases. Among other findings, haematuria can be a major sign of urinary tract and renal disease. Haematuria can also be physiological because the condition is intermitted (e.g. vigorous exercise, menstrual contamination) or due to hereditary predisposition (e.g. benign familial haematuria) [1, 2].
In case of pathological haematuria, the shape of the RBC is of special importance because it can give a hint to the source of bleeding. Locating the source of bleeding allows the differentiation of post-renal from renal haematuria and whether to refer the patient to a urologist or a nephrologist. Two main types of RBC can be found in urine sediments: isomorphic and dysmorphic RBC, indicating non-glomerular and glomerular bleeding, respectively [1, 3].
Isomorphic (also known as eumorphic) RBC mostly appear as round or biconcave disc shaped cells with a smooth surface and a rather uniform appearance. Dysmorphic RBC, on the other hand, have irregular shapes and contours and a broad spectrum of morphologic appearances [3] (they will be explained in more detail in the calendar in November).
Isomorphic RBC, a cell population similar in size and shape, indicate a post-renal non-glomerular haematuria, i.e. bleeding from the renal pelvis, ureters or bladder.
Additionally, morphology and haemoglobin content of RBC can also vary depending on pH, specific gravity and osmolality of the urine sample and delayed analysis of the specimen. In hypertonic urine, RBC begin to shrink to crenated shapes, such as echinocytes. An echinocyte is an RBC with many small, evenly spaced thorny projections, resembling a thorn apple. In contrast, RBC start to swell in dilute or hypotonic urine up to the point that the cell membrane ruptures and RBC gradually leak their haemoglobin. These empty membranes are known as ghost erythrocytes or shadow cells [1]. Increased lysis of RBC occurs in urine with a specific gravity below 1.010 and alkaline pH. Lysis processes are often observed if the specimen remains at room temperature for a prolonged time, since the pH can become alkaline due to the growth and metabolic activity of bacteria. Such morphological variations allow no reliable statement regarding the origin of the RBC (summarised in [4]).
Scattergrams
References
[1] European Urinalysis Group of the ECLM (eds. Kouri T et al.) (2000) European Urinalysis Guidelines. Scand J Clin Lab Invest. Vol. 60. Supplement 231.
[2] www.ncbi.com: Genetic testing registry.
[3] Poloni JAT, Bosan IB, Garigali G, Fogazzi GB (2012) Urinary Red Blood Cells: Not Only Glomerular or Nonglomerular. Nephron Clin Pract. 120:c36-c41.
[4] Over S (2002) The Effect of Delay in Processing on Urine Particle Analysis. Sysmex J Int. Vol. 12 No. 1.